Adhesive capsulitis, or frozen shoulder, affects 2-5% of the general population and is characterized by pain and progressive loss of shoulder range of motion. Frozen shoulder onset can follow trauma to the shoulder, such as a fracture, surgery, or period of immobilization. Adhesive capsulitis can also have an insidious onset, with no prior trauma or injury to the shoulder. There are many established risk factors for the onset of insidious adhesive capsulitis. Of those, diabetics have been identified as having a significantly higher risk of development, severity, and recurrence of insidious onset adhesive capsulitis. In this article, we will help you understand what the term adhesive capsulitis is, what diabetes is, the causes and risk factors for these conditions, as well as what the literature is supporting in regards to the correlation between frozen shoulder and diabetes!
What is Adhesive Capsulitis?
Adhesive capsulitis (AC) is characterized by shoulder pain, stiffness, and loss of range of motion. Primary AC has an insidious onset and is absent of any preceding trauma or injury. Secondary AC is diagnosed when there is a known cause, such as onset after trauma to the shoulder like a fracture, surgery, or immobilization. The presentation of primary and secondary AC is the same. In both primary and secondary AC, individuals often experience a negative impact on their daily functioning, and symptoms can be so severe to restrict any shoulder motion at all! The recovery process often takes years, with an average span of 18-30 months with some experiencing full recovery of motion while others may never return to full shoulder range of motion (1).
The following are risk factors that have been identified for the development of primary, or insidious onset, adhesive capsulitis.
- Several autoimmune disorders, including diabetes and thyroid disorders
- Dyslipidemia and other metabolic conditions
- Hypertension and cardiovascular disease
- Increasing age
- Females
Diabetics appear to be particularly susceptible to AC. It has been estimated that AC affects 2-5% of the general population, whereas the incidence of AC in diabetics is estimated to be as high as 20% (2)! Furthermore, an individual who has had diabetes for a longer duration can expect worse AC outcomes (3).
Are You Currently Dealing With Ongoing Shoulder Pain?
The Shoulder [P]rehab Program is a physical therapist-developed, step-by-step program that teaches you how to optimize your shoulder health, and overcome shoulder pain from a myriad of issues, such as frozen shoulder. To learn more, click HERE!
Learn How To Assess And Improve Overhead Shoulder Mobility
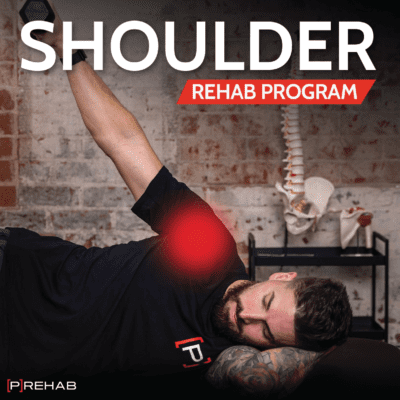
The Numbers On Diabetes
According to the American Diabetes Association, over 34 million Americans are currently living with diabetes, which is over 10% of the population. Each year, 1.5 million Americans are newly diagnosed with diabetes. Furthermore, in 2015, 88 million adult Americans were considered prediabetic, which is a staggering 34% of the population. Just looking at those already diagnosed with diabetes, we can expect 6.8 million of them to develop adhesive capsulitis at some point.
Type 1 Diabetes Vs. Type 2 Diabetes
Of the 34 million Americans with diabetes, only 1.6 million (or about 5%) of those are type 1 diabetics. Type 1 diabetes is a chronic condition in which the body attacks cells in the pancreas that produce the hormone insulin. Insulin is required to convert sugar into energy by allowing glucose to enter the body’s cells. Those with type 1 diabetes must take supplemental insulin via injections or insulin pumps on a daily basis to manage their blood glucose levels. The definitive cause of type 1 diabetes is unknown. Some hypothesized causes include exposure to viruses, or it may simply be due to one’s genetics.
Type 2 diabetics produce insulin, however, they may not make enough of it or their body develops resistance to the effects of insulin. This insulin resistance leads to high blood glucose levels. Some type 2 diabetics are able to manage their condition with diet and exercise, however, others may need to take oral medication to improve insulin action, and still, others may need to supplement with insulin, similar to type 1 diabetics. Contributing factors to type 2 diabetes onset include being overweight, fat distribution that is greater in the abdomen, physical inactivity, and increasing age.
LISTEN: CORTISONE SHOTS WITH DR. ALEX WEBER
The Stages & Progression of Adhesive Capsulitis
The typical progression of frozen shoulder includes gradual and progressively worsening pain in the shoulder, followed by a significant loss of shoulder motion. This progression can be broken down into three phases:
- Freezing: This is the most painful phase and can last anywhere from two to nine months. Patients experience diffuse and often disabling shoulder pain, which is typically worse at night. Later on, pain is also reported at rest. This is accompanied by increased stiffness and gradual loss of shoulder mobility.
- Frozen: This phase is characterized by the continued loss of shoulder motion, but typically with less pain. This phase typically lasts from four months up to one year.
- Thawing: This is the recovery phase, where a gradual return of shoulder motion is seen. Once in this phase, gaining full shoulder range of motion can take six months up to multiple years. In some cases, full range of motion is never achieved.
The Prehab membership is the anti-barrier solution to keeping your body healthy. Access state-of-the-art physical therapy, fitness programs, and workouts online in the comforts of your own home or gym! Taking control of your health with exercise & education from the palm of your hand has never been easier. Get access to 50+ programs, 100+ unique workouts, and 3000+ exercises to build your own workout routines. Trial it for free, and learn how to get out of pain, avoid injury, and optimize your health with [P]rehab!
What is the Link to Diabetes?
To begin to understand why the rate of idiopathic adhesive capsulitis is so much higher in diabetics, we first must look at the pathophysiology of frozen shoulder. The pathophysiology of adhesive capsulitis is still not entirely known or fully understood. One hypothesis is that increased inflammation within the glenohumeral joint capsule and synovial fluid triggers fibrotic changes and adhesions within the joint. Abnormal levels of cells that control collagen production result in imbalances between tissue breakdown, remodeling, and regeneration (2,4). Studies also show that subjects with AC have elevated levels of various types of inflammatory cytokines (4). With this information, it is theorized that AC stems from abnormal inflammatory processes that lead to fibrotic changes in the shoulder capsule. The pain associated with AC is attributed to the initial capsular inflammation, whereas the loss of range of motion is caused by the fibrotic changes and adhesions within the joint capsule.
Frozen Shoulder And Diabetes: Key Findings
A key feature of a frozen shoulder is the tightening and thickening of the glenohumeral joint capsule itself, along with adhesions within the joint and shrinking of capsular joint space. There is also a thickening of the rotator interval, a space at the anterosuperior aspect of the shoulder that is reinforced by ligaments and capsular fibers. A contracted and stiff coracohumeral ligament, which runs through the rotator interval, is also commonly found with adhesive capsulitis.
But Why Do All Of These Fibrotic Changes Occur?
There are many changes seen at the cellular and extracellular level with adhesive capsulitis. Altered levels and activities of fibroblasts, proteinases, and other extracellular components, which are responsible for collagen production and breakdown, scar tissue remodeling, and tissue regeneration, are found with adhesive capsulitis(2). Additionally, elevated levels of inflammatory markers are seen within the joint capsule (2). As previously stated, it is believed that the inflammatory changes lead to the fibrotic changes seen in the development of adhesive capsulitis.
So Why Do Diabetics Develop Frozen Shoulders At Such A High Rate?
A commonly accepted hypothesis for the increased incidence of adhesive capsulitis in diabetics is that systemically higher blood glucose levels lead to faster glycosylation. Glycosylation is the process by which sugar molecules are added to existing molecules, like proteins. Hyperglycemia or high blood sugar, essentially the definition of diabetes, results in increased formation of glycosylation products and advanced glycosylation end-products or AGEs (5). AGEs then go on to increase collagen, tendon, and ligament cross-linking resulting in stiffened and weakened structures (6). Furthermore, AGEs induce inflammatory changes through interactions with local cells and fibroblasts (6). Diabetics may also be more susceptible due to the chronic, systemic inflammation that accompanies both type 1 and type 2 diabetes.
Does Control Matter?
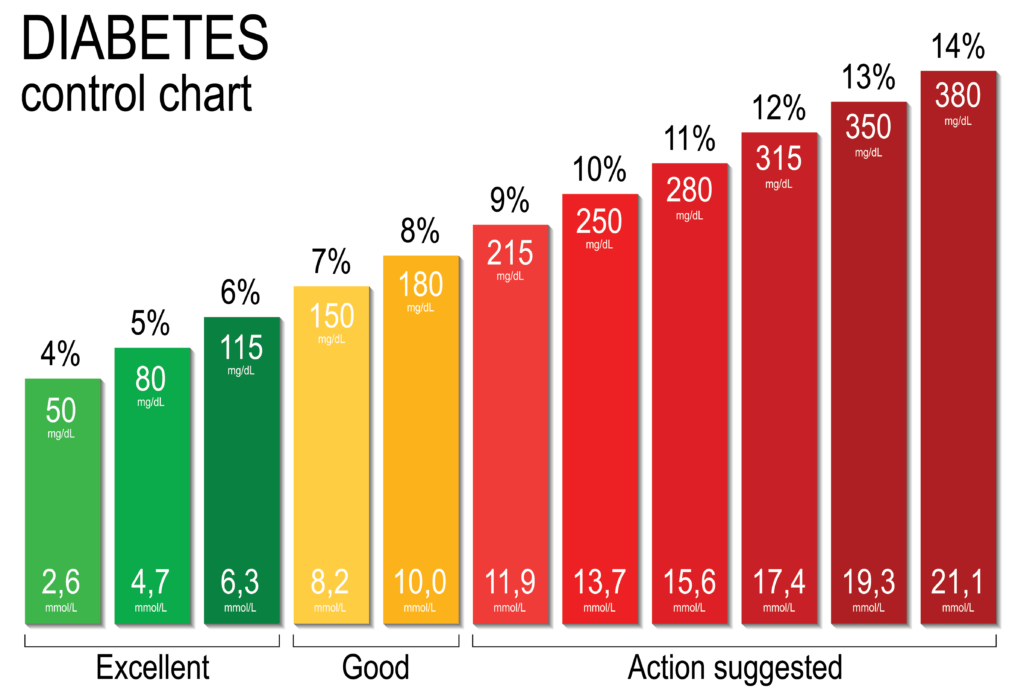
HbA1c is a short-term measure of average blood glucose control over the previous three months and is the most common way diabetics gauge their blood sugar control, outside of daily blood sugar testing. Some studies have shown that there is little correlation between HbA1c and adhesive capsulitis (7). However, one study by Chan et al (2017) created a variable known as “cumulative HbA1c” which looks at multiple HbA1c values over time to get a better estimate of the total disease burden that a diabetic experiences. They found that cumulative HbA1c had a significant positive correlation with adhesive capsulitis (8). Also significant was the effect size of cumulative HbA1c on adhesive capsulitis. Each time that an individual’s HbA1c was higher than 7, they found a 3% increase in frozen shoulder risk (8). Additionally, other studies have demonstrated a positive correlation between a longer duration of diabetes and adhesive capsulitis (7, 9). A study by Yian et al (2012) showed that individuals who had diabetes for greater than 10 years had increased odds of developing frozen shoulder versus those who had diabetes for less than five years (7). Therefore, it appears that diabetes management is important for adhesive capsulitis development and assessing a patient’s length of time with diabetes and total disease burden over years is a better predictor for adhesive capsulitis development than looking at a singular HbA1c score.
Frozen Shoulder And Diabetes: HBA1c Chart
Frozen Shoulder And Diabetes: Treatment & Outcomes
There is no consensus about the best course of treatment for individuals with frozen shoulder. This is especially true for diabetics with frozen shoulder, as they are consistently present with more severe and longer duration of symptoms, reduced responsiveness to conservative measures, and higher rates of recurrence (10).
Conservative Management: Studies show physiotherapy treatment leads to improvements in outcome scores, related to pain and function, for diabetics with frozen shoulder (11). For both diabetics and non-diabetics, physiotherapy group classes, passive exercises, and gentle, active shoulder exercises have been shown to improve outcomes in pain and function in the long-term (12,13,14). It should also be noted that recovery for most cases of adhesive capsulitis is spontaneous over time. However, studies report that anywhere from 20-50% of patients have long-lasting symptoms, including reduced range of motion (15,16).
Other conservative treatment measures include oral anti-inflammatory medications, oral corticosteroids, intra-articular steroid injections, and hydrodilatation. Oral steroid medication use, as well as corticosteroid injections, have shown to be beneficial for adhesive capsulitis outcomes, however, they can lead to persistent high blood sugars for diabetics. It should also be noted that the pain relief and improved function associated with steroid injections has been shown to only be of short-term benefit (17). For these reasons, the steroid route for diabetics may not be the best option for adhesive capsulitis treatment.
Hydrodilatation uses an ultrasound-guided local anesthetic injection into the glenohumeral joint. After the anesthetic, saline is injected into the joint to increase the capsular space and reduce the capsular contraction. Hydrodilatation has been shown to provide positive long-term benefits to patients with adhesive capsulitis and is often performed as an alternative to surgery (18,19,20). Despite the positive findings from a few studies regarding conservative treatment for diabetics with adhesive capsulitis, other studies have found that diabetic patients have higher rates of requiring surgical intervention and repeat hydrodilatation (21).
Frozen Shoulder Exercises
Below we will show you some great exercises that you can perform for frozen shoulder. The primary impairments related to adhesive capsulitis include pain and range of motion deficits. What is important is to match your irritability level with your intensity of exercise. For instance, for someone in the freezing stage of frozen shoulder, range of motion will be decreasing, yet pain will also be exponentially increasing. As a result, your exercises will be more passive, with less intensity. Examples include passive ranges of motion avoiding end range and working within what is tolerable based on your symptoms.
In contrast, once someone is in the frozen stage where the pain is decreased and ROM is also significantly impaired, one can begin working on their mobility and range of motion deficits by working more towards end range, longer hold times within end range, and so forth!
Frozen Shoulder And Diabetes: Pendulums
Sample Shoulder Rehab Program Exercise Video
- HOW: The pendulum exercise is a great beginner exercise to reduce pain and provide gentle motion for a frozen shoulder. The key to this exercise is to relax the shoulder as much as possible and allow the momentum from your hips and torso to provide the motion at the shoulder! To perform this exercise, begin with the non-affected arm on an elevated surface. While hinging over at your hips dangle the affected arm. You will move your arm in circles in this position initiating the motion from your body. If this is irritating your shoulder, you can stand upright. The less you hinge over the less stress on your shoulder.
- FEEL: You will feel the muscles in your shoulder and shoulder blade work with this exercise.
- COMPENSATION: Avoid over-stressing the affected arm. The muscles in the affected arm should very lightly be activated, use the momentum from your body to create a majority of the movement.
Standing Shoulder Cross Body Stretch – Posterior Cuff
Bring one arm up in front of you at shoulder height. Squeeze your shoulder blades together and then bring that arm across your chest while you use the other arm to slightly pull it more towards your chest. Hold that stretch for as long as prescribed.
Supine Shoulder IR
Sample Shoulder Rehab Program Exercise Video
Lying on your back, place one elbow 45 degrees out from your side. If 0 degrees was at your side, and 90 degrees was at shoulder height, 45 degrees would be in the middle of that. If needed, place a towel roll underneath your elbow. Bring your forearm up to make a “L” bend in your elbow. Grab onto the end of a dowel with that shoulder. The other hand will pull the dowel, which will rotate your shoulder down towards your belly button – keeping your shoulder as relaxed as possible. Hold that stretch for about 10 seconds, and repeat.
Side Lying Posterior Cuff Shoulder Stretch
Start by lying on your side. Bring the top leg up and bend at the knee. Let that knee relax on the ground. Straighten the bottom arm straight out in front of you. Place your other hand on the ground and turn your chest towards your arm until you feel a stretch in the back of your shoulder, rotate your bottom hand down.
Supine Shoulder Flexion PROM
Sample Shoulder Rehab Program Exercise Video
Begin laying face up with your fingers interlocked or held onto by the opposite arm. Initiate the motion with the non-affected arm, bring both arms as far overhead as possible. Keep the involved shoulder as relaxed as possible.
Operative Management
As previously stated, diabetics have an increased likelihood to require surgical intervention compared to non-diabetic patients (10). Two common operative procedures include manipulation under anaesthesia and arthroscopic release.
Manipulation under Anaesthesia (MUA) versus Arthroscopic Release
The outcomes are mixed for diabetics undergoing MUA, with some studies finding good long-term outcomes that are not significantly different from non-diabetic counterparts (22), but others finding poorer outcomes for diabetics (23). Upwards of 40% of diabetic patients following MUA require additional surgery, whether it is the same procedure again or an arthroscopic release (24). The MUA procedure has risks of fracture, labral, and rotator cuff damage as well as the potential for intra-articular damage. This risk is amplified if a repeat procedure must be performed, as is the case for many diabetics. Arthroscopic capsular release appears to be safer than MUA, with less risks of associated structural damage. Studies show that a capsular release results in improved range of motion and a reduction in symptoms in both the short and long term (25,26). It should also be noted that an arthroscopic release can be used to confirm the diagnosis of frozen shoulder, rule out other potential diagnoses, and provides a visual of the affected structures, including the coracohumeral ligament, glenohumeral capsule, and rotator interval. With the advantage of visualization of the affected structures with a capsular release, adequate release can be more readily provided.
READ: HOW TO ASSESS AND IMPROVE OVERHEAD SHOULDER MOBILITY
Prevention
Can adhesive capsulitis be prevented? Idiopathic adhesive capsulitis, because of its relatively unknown causation and poor understanding of development, can be hard to prevent. However, for diabetics, improving blood sugar control can reduce the risk, as increased disease burden from diabetes has been shown to positively correlate with frozen shoulder occurrence. In addition, looking at the risk factors associated with adhesive capsulitis, there are some that can be controlled for and managed to reduce an individual’s risk. Hypertension and cardiovascular disease as well as some metabolic conditions can be better controlled through diet, exercise, and weight management. According to the CDC, making small lifestyle changes can further negate these risks, such as getting more sleep, limiting alcohol consumption, and adopting healthy stress management techniques (27).
For anyone undergoing shoulder surgery, it is of the utmost importance to begin moving the surgical shoulder as soon as possible to prevent secondary adhesive capsulitis. Each surgeon will have their own protocol for immobilization and return to active and passive movements. A physical therapist is a post-op patient’s best friend for assisting with education and pain management as well as with the progression of rehabilitation, prevention of contractures, and return to normal function and beyond.
Closing Thoughts
Both type 1 and type 2 diabetics are at an increased risk of insidious onset adhesive capsulitis, with the risk increasing with longer duration and reduced control of diabetes. Possible mechanisms include alterations in inflammatory processes and increases in glycosylation products due to chronically elevated blood sugars and low level, systemic inflammation that often accompanies diabetes. At this time, there is no single agreed-upon treatment measure for frozen shoulder. Conservative measures, such as physiotherapy, are typically the first recommended course of action, followed by capsular release surgical intervention when conservative measures fail. As a means of prevention, well-controlled diabetes can lessen the total disease burden and reduce risks for insidious onset frozen shoulder. Additionally, improvements in lifestyle choices, such as performing daily exercise and weight management can further assist in indirect risk reduction.
Take Control of Your Shoulder Health
Movement from the shoulder girdle is what allows you to start to have access to feeding, grooming, and moving things around in your environment. Not that we like to play favorites or place one joints’ importance over another one but I think it’s safe to say, the shoulder is pretty dang important! It’s gifted with movement in all planes of motion which then burdens the joint to have stability and strength to control the mobility that it has. You will learn to use isometrics as a natural painkiller and utilize safe and effective strategies to restore function to the shoulder!
Disclaimer – The content here is designed for information & education purposes only and is not intended for medical advice.
About the author : [P]rehab
3 Comments
Leave A Comment
You must be logged in to post a comment.










I have frozen shoulder and at least 2 of the suggested exercises are impossible to do with a frozen shoulder.
Which two exercises are a problem?
Hi Lavonda!
Could you expand on your question here? Are you asking which exercises you should avoid if you are dealing with a frozen shoulder, or something different?
Best,
Team [P]rehab