“This blog is one of our ‘clinical pearls’, which is designed to assist clinicians in understanding exercise progressions for various clinical conditions. Throughout each of these clinical pearls, you will learn multiple ways to attack similar issues we all see when treating our patients. We also highlight many of our personal exercise library videos throughout these pearls, all of which you can gain access to as an exercise library member!”
Detailed Subjective: Training, Running Experience, Injury History
When starting to put together your pieces to the puzzle of differentially diagnosing runner’s knee, it is important to gather a detailed subjective regarding your patient’s running training as well as experience. Here are some key questions that you will want to ask:
What is your training volume? How many days are you running per week? What training surfaces do you run on?
We know that most running injuries occur due to OVERTRAINING. Oftentimes, simply educating your patients on appropriate training and programming can solve the issue!
If a runner is training on the same surface, it may make them more susceptible to injury. This is especially the case for uneven surfaces on the road if the runner is running on a slanted road, as well as downhill running in regards to runner’s knee, as this can create moment arm changes at the hip and knee, placing more stress and tension on the attachments of the IT band as well as the patella.
Have you had any previous injuries from running or outside of running?
Previous injuries are also a risk factor for recurring running injuries. It also may give you perspective on a patient’s movement impairments, running technique, etc. when moving forward with your evaluation. Common injuries to screen for include plantar fasciitis, stress fractures, posterior tibial tendinopathy, Achilles tendinopathy, runner’s knee, hip tendinopathy, or low back pain.
How long have you been running?
If someone is new to the sport of running, he or she may need more guidance in regards to running technique, proper training techniques, and how to build their body the right way for the sport.
What footwear do you utilize? Do you keep track of how often you change your running shoes?
Research is conflicting in regards to if shoe type truly matters in regards to preventing running injuries. However, research has shown that as the wear and support decrease on a shoe due to increased mileage, there is an increase in the amount of ground reaction force (GRF) that the body undergoes, which can lead to injury.
There is variability in regards to how often to change footwear, with most research agreeing around 300-500 miles depending on how quickly one wears down their shoes. Moreover, educating patients to try and have 2 pairs of shoes they can interchange throughout their training helps improve the lifespan of shoes.
The Ultimate Resource For Educating and Programming For Your Patients
Are you searching for a better way to provide education and exercise programming for your patients? The [P]Rehab Exercise Library is the best library available to the public that can optimize the resources you are providing for your patients and clients! Click HERE to gain access today.
What Is The Root of the Issue?
Before even starting with the rehab process for an individual with runner’s knee, you must figure out the root of the issue. From a pathophysiology perspective, we know that two of the most common causes of this condition include iliotibial band friction syndrome and patellofemoral pain syndrome. That is not to say that these pathologies are not able to occur simultaneously, as this occasionally is the case.
Here are some (not all) of the movement screens I like to utilize when evaluating runners:
Single Leg Squat To Chair Endurance Test
Sample [P]Rehab Exercise Library Assessment Video
Movements to keep an eye out for include: Knee valgus, excessive forward trunk lean, early heel rise, and poor eccentric control
Side Plank Endurance Test
Goal I shoot for initially is 20 seconds, and also if they can abduct the opposite hip
Lateral Step Down Endurance Test: Look for similar compensations you may see with single leg squat to chair
Single Limb Stance Opposite Hip Flexed and Eyes Closed: This gives me the ability to quickly screen the patient’s joint proprioception and foot positioning in single limb stance, which is heavily demanded during running.
Foot Posture Index: This will help you assess foot positioning and help you gather more information objectively when going through your examination process. You can find access to the Foot Posture Index HERE!
Single Leg Bridge Endurance Test: This is a great test to look for asymmetries with single limb positioning as well as motor control of the glutes
Functional Squat (unloaded and loaded): Look for any compensations such as weight shift towards weaker/uninvolved side, excessive posterior pelvic tilt, limited squat depth (mobility issue at ankle and/or hip), early heel rise, or forward trunk learn
Open Kinetic Chain (OKC) and Closed Kinetic Chain Ankle Dorsiflexion Range of Motion:
https://vimeo.com/38392670
Important to assess ankle dorsiflexion and if limited it may lead to compensations in runners.
Phase 1: Put Out The Fire
The first step in rehabbing runner’s knee is putting out the fire. We do not want to load the knee right away but work around it the best we can. A runner may need to stop their training entirely and purely focus on rehab in this first phase. This is a key part of your education, and ensuring the patient is fully bought in. It is perhaps the most challenging part of the rehab process. In addition to starting exercises to build strength, stability, and motor control of the core and lower extremities, there are also active release techniques that can be performed to help calm down the irritation around the knee.
Here are the Clinical Pearls of phase 1:
Dynamic Mobility: Place emphasis on addressing any flexibility deficits of the lower quarter, and if you are going to educate runners on foam rolling the IT band, make sure you teach them the RIGHT way! This is further described below.
Proximal Strengthening: Starting with some strengthening of the core stabilizers and hip musculature is great in phase 1. Mostly stick to exercises that do not place a large amount of stress on the knee joint. This will be saved for the later phases.
Don’t Forget The Quad: The quadriceps as we know is a key stabilizer to our patellofemoral joint. We know strengthening the hips is the sexy thing to do in knee rehab; however, we can’t neglect our quadriceps! This is especially important if you notice a runner may be having tracking issues, either when loaded or even unloaded.
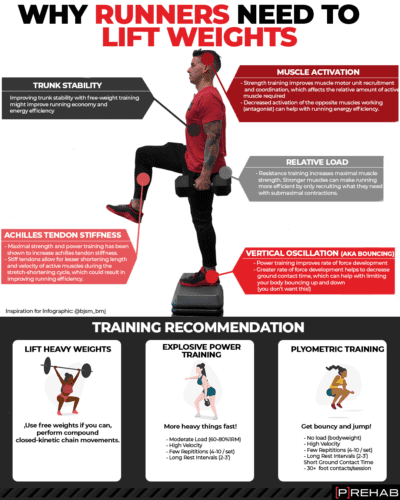
Why Runners Need To Do Strength Training
Phase 1 Dynamic Mobility
If there are any mobility deficits, you definitely want to address them early. Common areas of the lower extremity that are limited in mobility for individuals with runner’s knee include hip flexors (rectus femoris and iliopsoas), tensor fascia lata (TFL), hip rotators, hamstrings, and the gastrocnemius/soleus complex. In regards to stretching, research has not supported that static stretching reduces the risk of injury.
However, all runners should be educated in a dynamic movement routine prior to running. Just like any other activity, we want to prime our body for the activity we are going to do, whether that be bench pressing, Olympic weight lifting, or running.
This is one of my favorite ways to bias rectus femoris muscle length.
You can also have the patient place the back foot on a chair if they respond better to that body position versus using a strap as shown in this video.
The iliopsoas originates on the vertebral bodies of the lumbar spine, and inserts onto the lesser trochanter of the femur.
By elevating the arms and even adding a side bend of the lumbar spine to the opposite side of the hip you are stretching will help lengthen this muscle even further.
Great cue: Think about tilting your pelvis backward as well as pulling your rib cage away from your pelvis to create more movement and mobility.
Best Stretches After Running
Phase 1 Proximal Strengthening
Starting with proximal strengthening during the initial phase when the knee is still irritated is a great start. We know that hip and core deficits play a large role in knee pain with runners.
The clams exercise will promote muscle activation of our gluteus medius, as well as our gluteus maximus, which performs not only hip extension but external rotation.
Although the clamshell is a good exercise that you can start with, it is NOT the end all be all, best exercise for gluteus medius strengthening. The bigger bang for your buck glute med exercises involves more load, as we will discuss later on.
Strengthening of the gluteus maximus will help with the prevention of femoral adduction and internal rotation during mid-stance of running, which can place more unwanted stress at the knee.
The bridge exercise will also promote activation of the gluteus maximus.
We have an ENTIRE CLINICAL PEARL dedicated to Bridge Progressions, where you can learn more progressions of the bridge!
Establish their muscle firing pattern: With this movement, when you are educating a runner on how to perform this, pose the question first: “What area of your body do you feel is working the hardest?” That way before giving any cues or feedback, you can get an idea of the patient’s motor control and activation responses from their musculature when performing a bridge. The response will be one of the following:
- My Back: Compensation often seen when the posterior chain is inhibited and individuals overarch at their low back to compensate
- The back of my thighs: This may be due to either inhibition of the glute max, weakness of the glute max, or an increased lever arm of the hamstrings if the heels are too far from the buttock. This can be easily fixed by having the patient move their heels closer to their butt.
- The front of my thighs: The quads are a secondary mover during the bridge, but should not be the prime mover. Usually is due to quad dominance and/or posterior chain deficits
- My Butt: This is what we want!! If the patient feels that on their first try, there will not be much cueing you have to do besides telling the patient to do a bunch more reps!
HIGHEST GLUTE MED EMG ACTIVITY! You can read more about the best exercises for glute med activation HERE!
Sample [P]rehab Exercise Library Video
Do NOT neglect core stabilization with your runners. Dead bugs are an excellent way to work on promoting stiffness throughout our spine, which is very important during running to improve economy!
The Prehab membership is the anti-barrier solution to keeping your body healthy. Access state-of-the-art physical therapy, fitness programs, and workouts online in the comforts of your own home or gym! Taking control of your health with exercise & education from the palm of your hand has never been easier. Get access to 50+ programs, 100+ unique workouts, and 3000+ exercises to build your own workout routines. Trial it for free, and learn how to get out of pain, avoid injury, and optimize your health with [P]rehab!
Phase 1 Quadriceps Strengthening
If a runner is suffering from ITBFS, you may need to start quad strengthening within a shorter range of motion to avoid compression and/or friction of the IT band over the lateral femoral condyle/gerdy’s tubercle (its insertion point). Straight leg raises and short arc quads are a good place to start to promote quad activation within a shorter range.
Phase 2: Re-Exposure and Progressive Loading
Now that we have put the fire out, Phase 2 will consist of progressions of more stability and strengthening exercises, with a focus on single limb stability, which is essential when rehabbing runners.
The posterior lunge is a great start for individuals with runner’s knee if the knee is still irritated, as it will still put some load through the knee, but a greater emphasis on the hip musculature.
The trunk will flex forward naturally to keep your center of mass on the box, thus utilizing the glutes/hip more in addition to shortening the lever arm on the knee.
The forward step is one of the best exercises for runners. This exercise is very functional and translates to the coordination needed for running, works on both concentric and eccentric muscle contractions, and promotes unilateral weight-bearing to meet the demands of running.
When working on the forward step up, be sure your runners start with a lower step height, as compensations are often incorporated into movements with this exercise. Once they demonstrate very good single limb stability, eccentric control, joint proprioception, and strength, the following progressions can be made:
Higher Step Height: The higher height will require the lower extremity to go through a further range of motion, promoting more strength and stability benefits
Addition of weight – I am a proponent of a weighted vest if accessible to still work on arm swing while accomplishing axial loading, but if not, a barbell or dumbbells are also great
The captain morgan is an excellent way to target the hip abductors and external rotators with single limb loading.
The addition of the physioball will add more stabilization requirements throughout the core and lower body due to it being an uneven surface. If it is too challenging for your patient, start with a simple hip ER isometric against the wall, utilizing a fixed surface.
Running Strength Programming Low Hanging Fruits
Here are some principles to consider when programming strength training for runners:
The majority of strength training should be done during a more anaerobic focused running schedule, as strength and power are more closely associated with this system. This would include interval training, sprints, fartlek runs, and other workouts that incorporate utilizing lactate thresholds, VO2 max, and our phosphagen/glycolytic energy systems.
The myth of high reps and low resistance for runners simply is WRONG! Just like any other athlete, runners NEED LOAD!! Do NOT be afraid to load your runners.
When training endurance athletes, focus on neural adaptation training for runners with higher intensities and fewer reps. This will emphasize adaptations of our nervous system for running while not prioritizing muscle hypertrophy as the primary focus. This is more so implicated for competitive endurance runners who want to maximize their running economy by competing at a lighter body weight.
Closing Thoughts
Part one of this clinical pearl focused on gathering a detailed subjective history, establishing rapport and buy-in from your runners, and how to start rehabbing by putting out the fire. Address the impairments that you find in your initial evaluation and utilize those findings to guide your treatment plan. Work ‘around the knee’ by addressing proximal strength and/or core stabilization deficits as well as mobility impairments. From there, the graded exposure and beginning to load the knee is where the next progressions will be. In part 2, we will transition towards advanced rehab progressions and getting your runners back to the sport they love!
Take The Challenge Out Of Creating Programs For Your Runners
The [P]Rehab Exercise Library is the best library available to the public that can optimize the resources you are providing for your patients and clients! Click HERE to gain access today.
Clinician
Sherif Elnaggar, PT, DPT, OCS, SCS
[P]rehab Head of Content
 Sherif graduated from Temple University with a Bachelor’s of Science Degree and a concentration in Kinesiology. He then received his Doctorate of Physical Therapy Degree from DeSales University, graduating with honors of the professional excellence award and research excellence award. After his graduate studies, he served as Chief Resident of the St. Luke’s Orthopedic Physical Therapy Residency Program. Sherif is a Board Certified Orthopedic Clinical Specialist. Sherif focuses on understanding how movement impairments are affecting function while also promoting lifestyle changes in order to prevent recurrences of injury. His early treatment interests include running related injuries, adolescent sports rehab, and ACL rehab in lower extremity athletes. He also has been involved in performance training for youth soccer players. Outside of working as a physical therapist, he enjoys traveling, running and cycling, following Philadelphia sports teams, and spending time with his family.
Sherif graduated from Temple University with a Bachelor’s of Science Degree and a concentration in Kinesiology. He then received his Doctorate of Physical Therapy Degree from DeSales University, graduating with honors of the professional excellence award and research excellence award. After his graduate studies, he served as Chief Resident of the St. Luke’s Orthopedic Physical Therapy Residency Program. Sherif is a Board Certified Orthopedic Clinical Specialist. Sherif focuses on understanding how movement impairments are affecting function while also promoting lifestyle changes in order to prevent recurrences of injury. His early treatment interests include running related injuries, adolescent sports rehab, and ACL rehab in lower extremity athletes. He also has been involved in performance training for youth soccer players. Outside of working as a physical therapist, he enjoys traveling, running and cycling, following Philadelphia sports teams, and spending time with his family.
Disclaimer – The content here is designed for information & education purposes only and is not intended for medical advice.